Uterine Cancer :
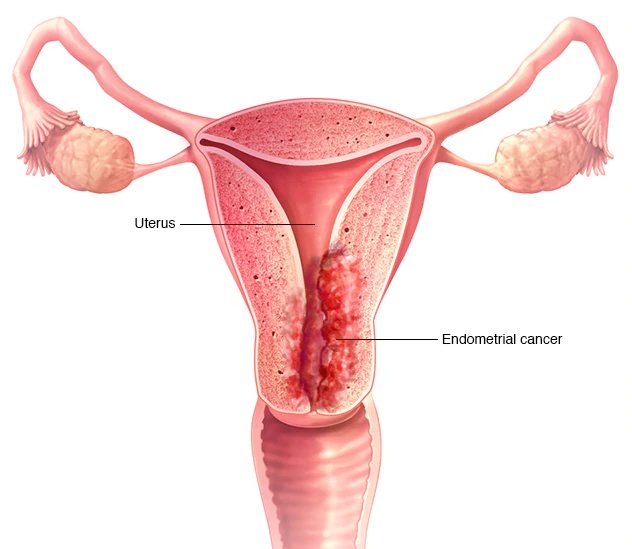
Uterine cancer is a very general cancer which develops in the woman’s reproductive system called as Uterus or Womb. Uterine cancer is also known as Endometrial cancer because it develops in the lining of the uterus, called as Endometrium. Generally, the risk of Uterine cancer in women grows with age, especially in those women who are going through or who have gone through the menopausal stage.
Uterine cancer grows when healthy cells in the uterus mutate and grow beyond control starts to convert in a tumour which can either be cancerous or benign. A cancerous tumour is malignant, means it can originate and expand to other parts of the body. A benign tumour can develop but normally doesn’t spread to other parts of the body.
Non-cancerous conditions of the uterus include :
Types of Uterine Cancer:
There are 2 major types of Uterine Cancer:
Adenocarcinoma:
Adenocarcinoma develops from cells in the endometrium. This cancer is commonly called Endometrial cancer. Treatment for Endometrial cancer depends on the extent of the spread of tumour into the uterus, and the stage or extent of the disease. Rare subtypes of uterine adenocarcinomas include serous, clear cell, and carcinosarcoma. Carcinosarcoma is a mixture of adenocarcinoma and sarcoma.
Sarcoma:
Sarcoma Uterine cancer develops in the connective tissues of the uterine glands or in the myometrium also known as Uterine muscle. About 2% to 4% women are affected by Sarcoma Uterine cancers. Secondary types of Endometrial sarcoma involves endometrial stromal sarcoma, leiomyosarcoma, and undifferentiated sarcoma.
Risk Factors of Uterine Cancer:
The risk of Uterine cancer may develop in women due to the following factors:
Signs and symptoms :
Women with uterine cancer do not have any of these changes. Or the cause of a symptom may be a different medical condition that is not cancer. Sometimes Women with uterine cancer may experience the following symptoms or signs.
Sometimes Women with uterine cancer may experience the following symptoms or signs.
The most common symptom of endometrial cancer is abnormal vaginal bleeding, ranging from a watery and blood-streaked flow to a flow that contains more blood. Vaginal bleeding during or after menopause is often a sign of a problem.
If a woman is diagnosed with Uterine cancer, then palliative care or supportive care treatment is given to the patient immediately after the diagnosis and is continued throughout treatment.
Symptoms of a tumour in the uterus usually affects both premenopausal and postmenopausal women.
Other common symptoms of endometrial cancer include:
For most women with uterine sarcoma, unusual vaginal bleeding or spotting is the most common symptom.
Other common symptoms of uterine tumours include:
Diagnosis of Uterine Cancer
Doctors have to perform many tests (imaging tests such as CT scans) or Biopsy for the diagnosis of cancer. Imaging tests like CT scans can show if the cancer has spread. Based on the test reports, Doctors can decide which best treatments could work for the patient.
Biopsy is the most authentic test for the doctor as it shows the location of the cancer in the body. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. The doctor may suggest other tests for the diagnosis only in case if a biopsy is not possible.
The other tests also may be used to diagnose uterine cancer:
A) Pelvic examination:
The doctor examines the uterus, ovaries, rectum, and vagina to check for any abnormal findings. Sometimes, in a Pap test, abnormal glandular cells are found, which are caused by uterine cancer.
B) Endometrial biopsy:
A biopsy is the procedure in which a small piece of tissue is removed. This sample is sent to the pathology lab and the pathologist analyses the sample under a microscope. A pathologist interprets laboratory tests and evaluates the cells and tissue samples to diagnose disease. In Endometrial biopsy, a very thin tube is used by the doctor to remove a small sample of tissue. In this process the tube is placed into the uterus through the cervix, and the tissue is removed with suction. Post the Biopsy, the woman may get cramps and vaginal bleeding. The doctor may prescribe the drug called as nonsteroidal anti-inflammatory drug (NSAID) which can reduce the symptoms. Only an Endometrial biopsy can make accurate diagnosis of Uterine Cancer.
C) Dilation and curettage (D&C):
D & C is a process in which tissue samples are removed from the uterus. During the procedure, the woman is given anaesthesia to block the sensation of the pain. D&C is normally combined with a hysteroscopy during the procedure which helps the doctor to view the lining of the uterus. In the hysteroscopy procedure, a thin flexible tube which has a light mounted on it is inserted by the doctor through the cervix into the vagina and uterus. During a biopsy or D&C, the endometrial tissue is removed, and the sample is sent to the pathology lab which is examined by the pathologist for checking the cancer cells, endometrial hyperplasia, and other conditions.
D) Transvaginal ultrasound:
Sound waves are used in ultrasound to create a picture of internal organs. In transvaginal ultrasound procedure, an ultrasound wand is inserted into the vagina and pointed at the uterus to click the images. If the thickness of the Endometrium is high, then the doctor may decide to perform a biopsy.
E) Computed tomography (CT or CAT) scan:
In Computed tomography (CT) scan, the images of the internal body are taken using x-rays from different angles. A computer merge these pictures into a detailed, 3-dimensional image which shows if there is any abnormalities or tumours. In a CT scan the tumour’s size can be measured. Sometimes, before the scan, a special dye called a contrast medium is given to deliver satisfactory info on the image. This dye can be inserted into a patient’s vein or even can be given as a pill or in the form of liquid to swallow.
F) Magnetic Resonance Imaging (MRI):
In MRI, magnetic fields are used to bring out detailed images of the body. Tumour’s size. can be measured with MRI. To create a clearer picture, alike CT scan, a special dye called a Contrast medium is given as intravenous or orally before the scan. If there is an inclusion of hormone management in the treatment plan, then MRI plays a great role in getting detailed images. In the women having low-grade uterine cancer, MRI is many times used in to examine the growth of cancer into the wall of the uterus. The MRI reports can discover whether a woman’s fertility can be preserved.
Stages of Uterine Cancer :
Cancer Staging is the method in which one can check the location of the cancer, its spreading and verifying the impact of cancer on other body parts.
Based on the information of samples of tissue from the surgery the Doctors go for diagnostic tests to locate the stage of the cancer. Unless the surgery is performed to remove the tumour, the staging cannot be completed until all the tests are done. The Uterine Cancer stage makes easy for the doctor to choose the type of best treatment that can be given predicting a woman's prognosis in which there is the chance of recovery. In case of Uterine cancer, the staging system is used which is developed by the International Federation of Obstetrics and Gynaecology (FIGO)
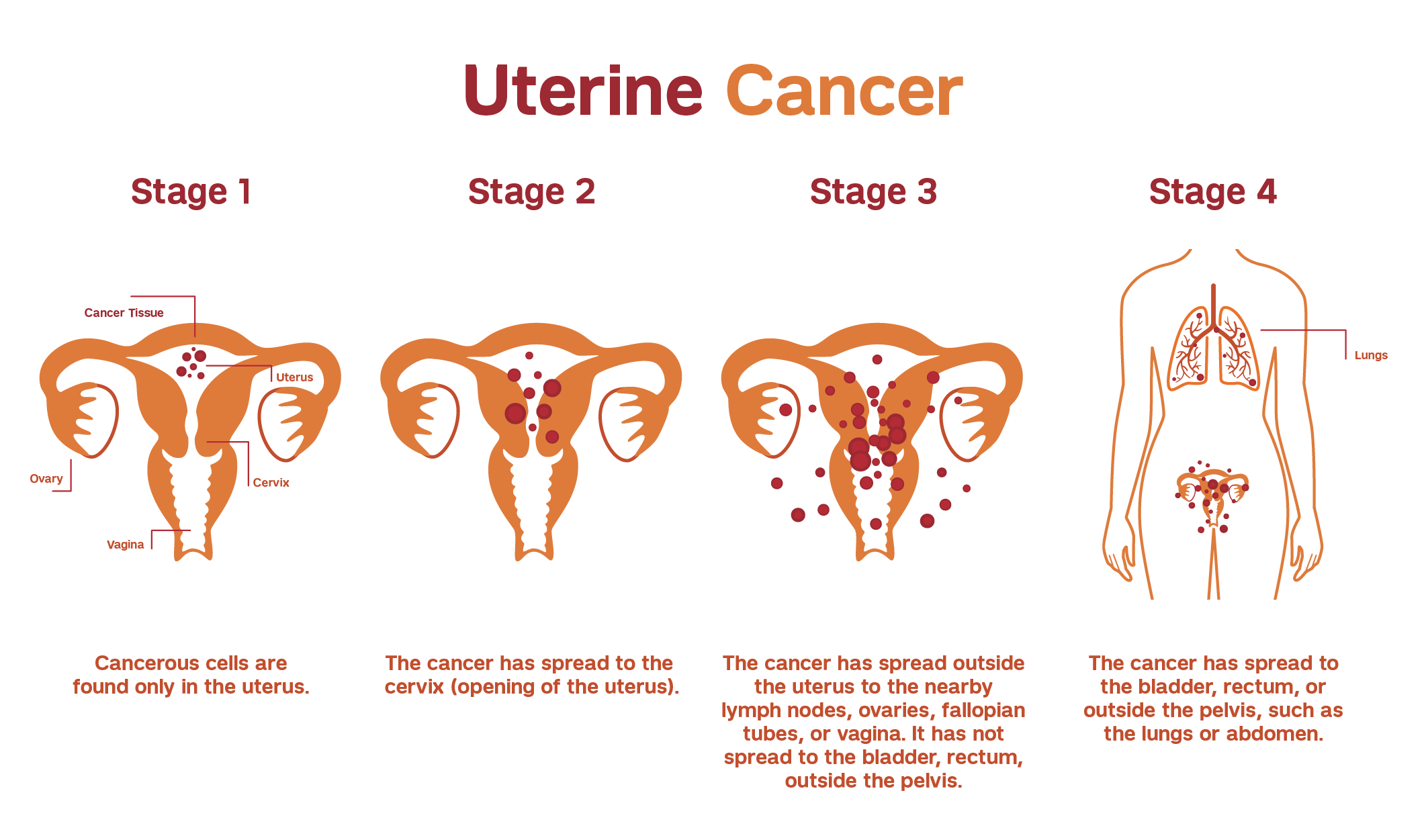
FIGO stages for uterine adenocarcinomas:
The FIGO stage offer a simple way of giving information about the cancer, helping the doctors to work together to plan the best treatments. Doctors decides the stage of endometrial cancer sing using the FIGO system.
Stage I :
The cancer is found only in the uterus or womb, and it has not spread to other parts of the body.
Stage II :
The tumour has spread from the uterus to the cervical stroma but not to other parts of the body.
Stage III:
The cancer has spread beyond the uterus, but it is still only in the pelvic area.
Stage IV :
The cancer has metastasized to the rectum, bladder, and/or distant organs.
Treatment for Uterine Cancer:
Treatment and suggestions by the doctor is based on various factors like the type of Cancer, stage of cancer, its prospective side effects, overall health of the patient, their age, and personal preferences. During the treatment, these factors will have to be considered to check the fertility condition of the woman to bear the child.
The treatment of Uterine cancer is done by 1 or a combination of treatments which includes surgery, radiation therapy, and systemic treatments using medications. Doctors majorly recommend these cancer treatments Combinations but usually depend on the stage and condition of the cancer.
A) Surgery:
Surgery is the process of removing the tumour and few surrounding healthy tissues, called a margin. The surgery of Uterine Cancer is performed by a Surgical gynaecologic Oncologist, a doctor who is specialized in treating gynaecologic cancer. Generally, Surgery is the first treatment used for uterine cancer.
Common surgical procedures for uterine cancer include:
B) Radiation therapy:
Radiation therapy is the use of high-energy x-rays or other particles to destroy cancer cells. A doctor who specializes in giving radiation therapy to treat cancer is called a radiation oncologist. A radiation therapy regimen, or schedule, usually consists of a specific number of treatments given over a set period of time. Radiation therapy can be delivered externally or internally. External-beam radiation therapy uses a machine outside the body to deliver radiation to the pelvic region or the area designated by your radiation oncologist. Radiation can also be delivered internally. This form of radiation is called brachytherapy. External-beam radiation therapy can be given alone or in combination with brachytherapy. For some people, brachytherapy alone will be recommended. The most common type of radiation treatment is external-beam radiation therapy.
The radiation therapy is most often given after surgery to destroy any remaining cancer cells. Radiation therapy is occasionally given before surgery to shrink the tumor. If a woman cannot have surgery, the doctor may recommend radiation therapy instead.
Options for giving radiation therapy to treat uterine cancer may include radiation therapy directed towards the whole pelvis and/or applied only to the vaginal cavity, often called vaginal brachytherapy. Some women may be able to have vaginal brachytherapy instead of radiation to the pelvis if they have a grade 1 or 2 cancer that has spread through half or more of the myometrium or if they have a grade 3 cancer that has spread through less than half of the myometrium.
For some women, radiation therapy to the pelvis may be the best option to help prevent a return of the cancer. These women include those with a grade 3 cancer that has spread through half or more of the myometrium; those with a cancer of any grade that has spread to tissue in the cervix; and those with a cancer that has spread outside the uterus to nearby tissue or organs. In these situations, a woman may need only radiation therapy after surgery, only chemotherapy, or a combination of radiation therapy and chemotherapy. Your doctor will be able to help you figure out which of these options is right for you.
Radiation therapy to the pelvis may also be considered for some women with grade 1 or 2 cancer that has spread through half or more of the thickness of the myometrium, depending on factors such as age and whether the cancer has spread to blood or lymphatic vessels.
C) Chemotherapy:
Chemotherapy, which uses drugs designed to destroy cancer cells and shrink tumors, is an important part of treatment for many uterine cancer patients at CTCA, whether they have received previous chemotherapy treatments elsewhere or not.
Our gynaecologic oncologists treat uterine cancer with a comprehensive and personalized approach, which may include using various chemotherapy drug combinations.
Another uterine cancer treatment option we offer is hormone therapy, which slows the growth of cancer cells by reducing hormone levels in the body. This type of hormone therapy may be used alone or in combination with surgery and other therapies, depending on the type and stage of the disease.
At CTCA, we use innovative approaches in uterine cancer hormone therapy, attacking the disease on multiple fronts with a variety of drugs. A common regimen may include progestins, which are a synthetic form of progesterone that slows or stops the growth of uterine cancer cells. Other drugs reduce estrogen levels or block its effect on cancer cells, including tamoxifen and gonadotrophin releasing hormone agonists.
Our supportive care services help manage side effects of cancer hormone therapy, like hot flashes and low libido. We anticipate side effects by focusing on prevention, and manage them with a variety of approaches if they do occur. All of this is integrated into your overall uterine cancer treatment plan, with personalized support for you and your family.
D) Hormone therapy:
Hormone therapy is used to slow the growth of certain types of uterine cancer cells that have receptors to the hormones on them. These tumours are generally adenocarcinomas and are grade 1 or 2.
Hormone therapy for uterine cancer often involves a high dose of the sex hormone progesterone given in pill form. Other hormone therapies include hormone-expressing intrauterine devices (IUDs) and aromatase inhibitors (AIs), such as anastrozole (Arimidex), letrozole (Femara), and exemestane (Aromasin), which are often used for the treatment of breast cancer. An AI is a drug that reduces the amount of the hormone estrogen in a woman's body by stopping tissues and organs other than the ovaries from producing it. Hormone therapy may also be used for women who cannot have surgery or radiation therapy, or it can be used in combination with other types of treatment.
Side effects of hormone therapy may include fluid retention, increase in appetite, insomnia, muscle aches, and weight gain. Most side effects are manageable with the help of your health care team. Talk with your doctor about what you can expect.
E) Targeted therapy:
Targeted therapy is a treatment that targets the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. This type of treatment blocks the growth and spread of cancer cells and limits damage to healthy cells.
Not all tumours have the same targets. To find the most effective treatment, your doctor may run tests to identify the genes, proteins, and other factors in your tumour. This helps doctors better match each patient with the most effective treatment whenever possible. In addition, research studies continue to find out more about specific molecular targets and new treatments directed at them. Learn more about the basics of targeted treatments.
Targeted therapy for uterine cancer is available in clinical trials and, in some instances, as part of standard-of-care treatment regimens. Targeted therapy for uterine cancer includes:
Anti-angiogenesis therapy. Anti-angiogenesis therapy is focused on stopping angiogenesis which is the process of making new blood vessels. Because a tumour needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumour. Bevacizumab (Avastin) is a type of anti-angiogenesis therapy used to treat uterine cancer.
Mammalian target of rapamycin (mTOR) inhibitors. In endometrial cancer, mutations in a pathway called mTOR are commonly found. People with advanced or recurrent uterine cancer may be treated with a drug that blocks this pathway, such as everolimus (Afinitor). Other drugs that target this pathway are being studied, such as ridaforolimus and temsirolimus (Torisel), a targeted therapy approved to treat a type of kidney cancer called renal cell carcinoma.
Targeted therapy to treat a rare type of uterine cancer. Uterine serous carcinoma is a rare but aggressive type of endometrial cancer. About 30% of these tumours express the HER2 gene. In a phase II clinical trial, researchers found that trastuzumab (Herceptin) combined with a combination of chemotherapy was effective in treating these kinds of tumours. Trastuzumab is a HER2 targeted therapy mostly used to treat HER2-positive breast cancer.
F) Immunotherapy:
Immunotherapy, also called biologic therapy, is designed to boost the body's natural defences to fight the cancer. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function.
Uterine cancers with mismatch repair defects (dMMR; see Introduction) are more sensitive to immunotherapy. The immunotherapy drug pembrolizumab (Keytruda) is approved to treat tumours that have either high microsatellite instability (MSI-high) or dMMR, regardless of the tumour’s location in the body. Pembrolizumab can be used to treat uterine tumours with dMMR if other previous treatments have not worked.
A combination of Lenvatinib (Lenvima), a targeted therapy drug, and pembrolizumab is also approved to treat advanced endometrial cancer. This combination can be used to treat disease that is not MSI-high or dMMR, has not been controlled by systemic therapy, and cannot be cured with surgery or radiation therapy. Lenvatinib may cause high blood pressure.
Different types of immunotherapy can cause different side effects. Common side effects include skin reactions, flu-like symptoms, diarrhoea, and weight changes. Talk with your doctor about possible side effects for the immunotherapy recommended for you. Learn more about the basics of immunotherapy.


